My child has misshapen feet, is this normal?
– “What is it?”
What is it?
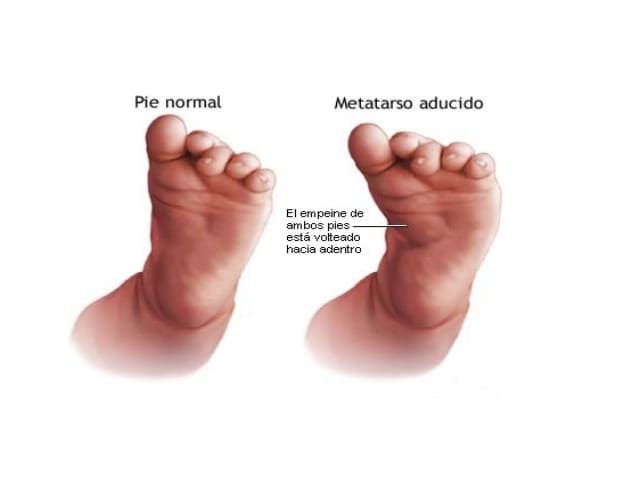
This is a congenitalmalformation of the foot at the level of the tarsometatarsal joint(commonly known as the Lisfranc joint)that affects the soft tissues. It frequently occurs in newborns, in whom, if identified early and treated correctly, it is resolved in the majority ofcases without the need for surgery, thus avoiding complications derived from this type of procedure that lengthen recovery times. it is resolved in the majority of cases without the need for surgery, thus avoiding complications derived from this type of procedure that lengthen recovery times. thus avoiding complications derived from this type of procedure that lengthen recovery times.
Metatarsus adductusis characterised by a disorder of forefoot alignment,with variable degrees of adduction and supination,and is often associated with a slight rearfoot valgus, a differentiatingaspect ofclubfoot (6-7).
How is it diagnosed?
Diagnosis is fundamentally clinical,a goodanamnesis and an appropriate physicalexamination are essential.. The contribution of complementary tests is less essential; it is not necessary to carry out radiographic tests on a regular basis in this type of pathology as they do not allow us to demonstrate forefoot mobility. However, it can be useful in advanced deformities to assess their severity and the effectiveness of treatment (8-9).
How is it classified according to its severity?
“In order to unify diagnostic and treatment criteria, as well as to anticipate a prognosis”, C. Martos Mora et al. propose a clinical-therapeutic classificationbased on a retrospective study of 87 patients with metatarsus adductus. They established three degrees of intensity of involvement: (5)
- – Grade 1: The deformity is mild.. Forefoot adduction only, no inversion occurs. The foot can be abducted passively or by stimulation of the peroneal musculature.
- –Grade 2: The deformity is semi-rigid.. Adduction and inversion of the forefoot. There is some convexity of the outer edge, concavity of the inner edge, normal longitudinal arch and prominent and palpable fifth metatarsal.
- – Grade 3: The deformity is more structuredand acquires a ‘kidney-shaped’ form,with oblique grooves in the midfoot region and increased internal longitudinal arch. Unlike grades 1 and 2, passive correction of the forefoot is not possible at this stage. (2) (4-5) (2) (4-5)
How is it treated?
In the mildest cases it resolves spontaneously and in the remaining cases, if it is not corrected,the child will have an uncomfortable gait with internal deviation of the toes, thus favouring falls and, in the long term, the development hallux valgus due to abnormal shoe fitting (6-7).
If it does not resolve spontaneously in the first weeks of life,conservative treatmentis carried out, which includes:casts, curved hypercorrection pads, splintsor bandages.. The time of correction will depend on the severity, it is certain that the deformity must be corrected before the child begins to walk.. If conservative treatment fails, or if the child is older than 4 years atthe time of diagnosis, surgical correction should be proposed.. The preferred technique appears to be an opening wedge osteotomy of the first cuneiform using a bone graft,in combination with a closing wedge osteotomy at the base of the second to fifth metatarsal (4) (10-11).
The general opinion isthat serial cast similar to those used in clubfoot are necessary, changing every 7 to 14 days for 1-3 months (12-13). In the experience of C. Martos-Mora et al (5), almost complete correction can be obtained withdaily bandaging in an average of only 15 days, witha maintenance splintbeing used afterwards to prevent the natural tendency of the foot to return to its original position. The advantages of bandaging and bracing would include, in addition to the shortened treatment period, the ease with which the child’s hygiene is carried out and the possibility of daily manipulation of the foot. In more structured cases, it isproposed to maintaincorrection by wearingstraight-fitting boots until 18 monthsof age(14).
It should be noted that the method of functional corrective bandaging is highlyeffective in the correction of metatarsus adductus foot. E. Utrilla Rodríguez et al carried out a retrospective study of 94 children born with this deformity and treated with this method, 68.1% achieved correction (4). It is advisable in cases of flexible metatarsus adductus to monitor the posture of children when sitting/sleeping as they can force the foot into a prolonged adduction position and this does not help correction. (15) (15)
In summary, treatment will depend on the degree of involvement being favourable when the foot is more flexible, within the first year. Sometimes the deformity is evident at birth, although in most cases, it is not detected until weeks or months later. Metatarsus adductus foot is a frequent reason for consultation associated with considerable family distress, and has a good prognosis.Early diagnosis is essential for proper management and outcome. (1-4)
Bibliography
-
Fishco W, Ellis M, Cornwall M. Influence of a Metatarsus Adductus Foot Type on Plantar Pressures During Walking in Adults Using a Pedobarograph. The Journal of Foot and Ankle Surgery. 2015;54(3):449-453
-
Williams C, James A, Tran T. Metatarsus adductus: Development of a non-surgical treatment pathway. Journal of Paediatrics and Child Health. 2013;49(9):E428-E433
-
Winell JJ, Davidson RS. The foot and toes. In: Kliegman RM, Stanton BF, St. Geme JW, Schor NF, eds. Nelson Textbook of Pediatrics. 20th ed. Philadelphia, PA: Elsevier; 2016: 674.
-
Utrilla Rodríguez E, Guerrero Martínez-Cañavete M, Albornoz Cabello M, Munuera P. Tratamiento del pie metatarso aducto con el método de vendajes funcionales correctores: estudio retrospectivo. Fisioterapia. 2016;38(5):229-234
-
Martos-Mora C, Gentil-Fernández J, Conejero-Casares J, Ramos-Moreno R. Metatarso aducto congénito: clasificación clínica y actitud terapéutica. Rehabilitación. 2012;46(2):127-134
-
Gómez MP, García JM. Enfoque terapéutico del metatarso aducto congénito. Medicina de Rehabilitación. 2000;13(3):29-31
-
Esteo I, Méndez LI, Gómez A, Muñoz Y, Díaz S, Devolx A, et al. Metatarso varo: ¿yesos o botas correctoras? Rev And Traum Ort. 2001;21(1):33-39
-
Reina M, Lafuente G, Trujillo P, Ojeda A, Munuera PV, Domínguez G. Metatarsus adductus: revisión y propuesta de tratamiento. Rev Esp Podol. 2006;17(1):18-23
-
Turner WA, Merriman ML, editores. Habilidades clínicas para el tratamiento del pie. Madrid: Elsevier; 2007
-
JE Herzenberg, RD Burghardt. Metatarsus aductus resistente: ensayo prospectivo aleatorizado de yeso versus ortesis. J Orthop Sci , 19 ( 2014 ) , págs. 250 – 256
-
L. Feng , M. Sussman. Osteotomía cuneiforme medial combinada y osteotomías metatarsianas múltiples para la corrección del metatarso aducto persistente en niños. J Pediatr Orthop , 36 ( 2016 ) , págs. 730 – 735
-
Jackson JF, Stricker SJ. Pediatric foot notes: a review of common congenital foot deformities. International Pediatrics.2003;18:133-40. —–2
-
Sass P, Hassan G. Lower extremity abnormalities in children. Am Fam Physician. 2003;68:461-8. —12
-
Calzadilla Moreira V, Castillo García I, Blanco Estrada J, González, Martínez E. Desviaciones torsionales de los miembros inferiores en ni˜nos y adolescentes. Rev Cubana Med Gen Integr.2002;5:355-61.
-
Iglesias L, Vallejo B, Crespo S, Fuentes S. Mala postura al sentarse y deformidad del metatarsu aducto. J.Am. Podiatr. Med. Assoc. 2009;99:174-7.